
According to the National Institute on Aging, older adults need more, not less, sleep as they age—7 to 9 hours each night. And women may need more sleep than men. But aging brings with it a number of challenges to sleep quality and duration. Can you actually remember when you last had a really good night’s sleep?
Sleep, glorious, often evasive, sleep is one of the pillars of good health, along with diet and exercise. Yet as we get older our sleep systems change, affecting our ability to fall–or stay–asleep.
Getting enough sleep is the best thing you can do for your health
Losing as little as one hour of sleep in a night can have a dramatic impact on your health. So says Dr. Matthew Walker, British scientist and professor of neuroscience and psychology at the University of California, Berkeley. Just consider the effects of the ‘global experiment’ that takes place twice a year and involves 1.6 billion people across more than 60 countries: daylight saving time.
In the spring, when we lose one hour of sleep, there are 24% more heart attacks the next day. In the autumn, when we can sleep an extra hour, heart attacks go down 21%. Most of us think little of losing an hour of sleep. Maybe we should think again.
Why a good night’s sleep is so important
Science is only beginning to understand the full extent of sleep’s essential role in brain and body health. We do know some of the reasons why getting the right amount of sleep is critically important for our health, especially as we age.
Sleep sweeps away toxins in the brain.
Research suggests sleep plays a housekeeping role that removes toxins that build up in the brain during the day. According to Dr. Maiken Nedergaard, a professor of neurosurgery at the University of Rochester, when we sleep, the flow of cerebrospinal fluid in the brain increases dramatically to wash away harmful waste proteins that build up between brain cells during waking hours. It’s like a dishwasher for the brain.
Sleep improves concentration and productivity.
A good night’s sleep improves problem-solving skills and enhances memory. It also supports key brain functions like cognition, concentration, productivity, and performance. Dr. Nedergaard explains that lack of sleep and the toxins that build up during the night could explain why we don’t think clearly after we have slept poorly. And, a lengthy sleep deficit can actually kill us. Poor sleep has also been shown to compromise brain function similar to having a drink or two.
Sleep heightens our immunity against illness.
Even a small sleep deficit can compromise the body’s immune function. Take this large two-week study that monitored more than 150 people to see who was most susceptible to catching a cold. Each was given nasal drops that contained a virus for the common cold. They found that those who slept less than seven hours were almost three times more likely to develop a cold than those who slept eight hours or more.
Sleep supports physical performance.
Sleep is necessary to carrying out physical activities at our best, whether we’re in a Zumba class or walking the dog. According to the National Sleep Foundation, research suggests that not getting enough sleep increases levels of the stress hormone, cortisol. It also decreases the production of the glycogen and carbohydrates that we store for energy during physical activity. In short, less sleep increases the likelihood of becoming tired, not feeling energetic, and finding it difficult to focus.
And if we don’t get enough sleep…
Not getting enough sleep increases our risk of a wide range of health issues, like high blood pressure, cardiovascular disease, diabetes, depression, and obesity.
We gain weight.
Sleep’s role in weight gain is linked to various factors, including hormones and how motivated we feel to exercise. When we don’t get enough sleep, we tend to eat more. Our bodies produce higher levels of ghrelin, the hormone that stimulates appetite, and lower levels of leptin, the hormone that suppresses appetite and signals we are full.A study of over 1,000 people found that those who slept fewer hours had 14.9% higher ghrelin levels and 15.5% lower leptin levels than those who got enough sleep. In addition, getting less sleep can lead to higher BMIs.
There’s a greater risk of heart disease and stroke.
A review of 15 studies found that those who don’t get enough sleep are at far greater risk of heart disease or stroke than those who sleep 7–8 hours per night.
- Type 2 diabetes. Poor sleep habits are strongly linked to problems with blood sugar levels. According to numerous studies, those who sleep less than six hours per night are at an increased risk of type 2 diabetes.
- Depression. About 90% of those with depression complain about sleep quality. Conversely, those with sleeping disorders like insomnia or obstructive sleep apnea report significantly higher rates of depression. Poor sleep is also associated with an increased risk of suicide in older adults.
- Inflammation. Getting less than, or more than, 7-8 hours of sleep per night has been shown to increase inflammatory markers in the blood, like C-reactive protein (CRP) and interleukin-6 (IL-6). These markers are linked to chronic diseases like heart problems, hypertension, and type-2 diabetes. Poor sleep has also been linked to long-term inflammation of the digestive tract, in disorders known as inflammatory bowel diseases.
Seven to nine hours is the sweet spot
According to Dr. Walker, a consistent seven to nine hours of sleep each night “is the single most effective thing we can do to reset our brain and body health each day.”
The quality of your sleep is just as important. This is affected in myriad ways: how long it takes to fall asleep; how often you wake during the night; how rested you feel the next day; or how much time you spend in the different stages of sleep.
Women may need more sleep than men
According to Jim Horne, a leading British neurologist and director of the Sleep Research Centre at Loughborough University, women need more sleep than men. This is attributed to women using their brains more actively than men—about 20 minutes more, reports Independent.co.uk.
The more of your brain you use during the day, the more of it that needs to recover. This translates into a need for more sleep.
“Women tend to multi-task—they do lots at once and are flexible and so they use more of their actual brain than men do. Because of that, their sleep need is greater,” says Horne.
For many of us, though, a good night’s sleep becomes more elusive with each passing year.
So how can we get a good night’s sleep?
It’s all about our sleep architecture
There’s much debate on whether we need less sleep as we get older. We need about the same amount of sleep throughout adulthood, between seven to nine hours. But as we age, we need more time to fall asleep. And once asleep we don’t sleep as well as when we were younger. It’s part of the normal aging process.
Although the total amount of time we’re asleep doesn’t change much, the way we sleep—what specialists call “sleep architecture”—does. We spend more time in the lighter sleep stages and less time in REM and deep sleep.
Sleep goes through four stages
There are two basic types of sleep: rapid eye movement (REM) sleep and non-REM (NREM) sleep. Each has specific brain waves and neuronal activity. At night our body cycles through the four stages of sleep several times. Increasingly longer, deeper REM periods take place as the clock moves toward morning. We typically experience all sleep stages during 90 minute sleep cycles.
During the three stages of NREM sleep we move from light sleep in Stage 1 to very deep sleep in stage 3.
Stage 1 NREM sleep is when we are falling asleep. Brain waves begin to slow from their daytime wakefulness patterns. This stage lasts several minutes.
Stage 2 NREM sleep is the light sleep before we enter deeper sleep. Our body temperature drops and our eyes stop moving. Brain waves slow and are marked by brief bursts of electrical activity. We spend more of our repeated sleep cycles in stage 2 sleep than any other.
Stage 3 NREM sleep is the deep sleep we need to feel fresh in the morning. Our heartbeat and breathing slow to their lowest levels. Muscles relax and it may be difficult for someone to wake us. Our brain waves become even slower. Stage 3 sleep occurs in longer periods during the first half of the night.
REM sleep first occurs about 90 minutes after falling asleep. Our eyes move rapidly from side to side behind closed eyelids. Mixed frequency brain wave activity becomes closer to that of wakefulness. Our breathing becomes faster and irregular, and our heart rate and blood pressure increase to near waking levels.
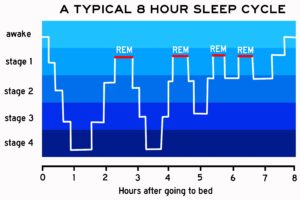
Most dreams occur during REM sleep. Our arm and leg muscles are temporarily paralyzed, all the better to stop us from acting out our dreams. As we age, we spend less time in REM sleep. Memory consolidation most likely requires both non-REM and REM sleep.
While you’re asleep, your body is hard at work. An article on Healthline.com lists a few of the processes taking place while you sleep.
- Your body rebuilds muscles you’ve worn down during the day and cleans away harmful plaques and waste produced in the brain. These are vital processes that keep both your mind and body running properly.
- Your mind processes and responds to important emotions and experiences from the day and commits them to memory. Your emotional responses are regulated by the amount of sleep you get. Being sleep deprived for just one night can increase your emotional response to negative feelings by 60%.
- A lack of sleep makes it difficult for your body to regulate essential things like appetite control, your immune system, good metabolic function, and your ability to maintain a normal body weight.
- Sleep plays an important role in regulating your circadian rhythm, or internal clock.
Two systems regulate our sleep and wakefulness
Circadian rhythms and homeostasis work together to regulate our sleep and wakefulness.
Circadian rhythms
These key rhythms follow a pattern each day to orchestrate our various bodily functions–sleep and wakefulness, body temperature, metabolism, and the release of hormones. They are regulated by certain parts of the brain, certain hormones (including melatonin), and environmental cues like temperature and light.
Experts believe that as we age our sleep rhythm signal becomes weaker. It becomes less effective in directing the body’s processes to synchronize with each other and with the day. Our body’s circadian rhythm changes, impacting our sleep. We become tired earlier in the evening and wake up earlier in the morning, so we still get seven or eight hours of sleep.
Sleep-wake homeostasis
Sleep-wake homeostasis reminds our bodies when we need sleep as well as regulates how deeply we sleep. Our need to sleep becomes stronger the longer we are awake. It also causes our bodies to sleep longer and more deeply after we have been deprived of sleep.
Factors that affect our sleep-wake needs include medical conditions, medications, stress, sleep environment, and diet. Perhaps the greatest influence is our exposure to light. Specialized cells in the retinas of our eyes process light. They tell the brain whether it is day or night and can change–advance or delay–our sleep-wake cycle. Being exposed to light can make it difficult to fall asleep or fall back asleep once awake.
A clear instance of the roles of circadian rhythms and sleep-wake homeostasis is witnessed in night shift workers. They often find it difficult to fall asleep when they go to bed, and also have trouble staying awake at work because their natural circadian rhythm and sleep-wake cycle have been disrupted. With jet lag, circadian rhythms become out of sync with the time of day when we fly to a different time zone. This creates a mismatch between our internal clock and the actual time clock.
Understanding the sleep-wake cycle is clearly essential to good health. It is so important that researchers Jeffrey C. Hall, Michael Rosbash, and Michael W. Young received a Nobel Prize for their work in the molecular mechanisms controlling circadian rhythm.
Sleep disorders are more likely as we get older
We run a greater risk of experiencing a sleep disorder as we get older. These can include sleep apnea, restless leg syndrome (RLS), periodic limb movement disorder (PLMD), and REM behavior disorder. Sleep apnea especially increases in women.
- Insomnia — As many as 44% of older persons experience one or more of the nighttime symptoms of insomnia at least a few nights per week. Insomnia may be chronic (longer than a month) or acute (last a few days or weeks) and is often linked to an underlying cause such as a medical or psychiatric condition.
- Snoring — Snoring disrupts the sleep of some 90 million American adults, 37 million of them regularly. And ladies, don’t point your finger at the men. Twenty-four percent of adult women are habitual snorers.
- Sleep apnea — Loud snoring can signal obstructive sleep apnea (OSA), a condition linked to high blood pressure and other health problems. With OSA, breathing stops–sometimes for as long as a minute. Oxygen levels in the blood drop, which alerts the brain and causes the sleeper to wake and resume breathing. Untreated sleep apnea increases the risk for cardiovascular disease, headaches, memory loss, and depression. Women over 50 may be more at risk for these disorders than men.
- Restless legs syndrome — Restless legs syndrome (RLS) is a neurological movement disorder characterized by an overwhelming need to move the limbs—mostly the legs. It becomes worse in the evening and makes it difficult to sleep through the night. RLS becomes more common with age, with about 10% of people in North America and Europe reporting symptoms. While people of any age can have RLS, the syndrome typically strikes older adults and affects women more often than men.
Health issues and life events can interfere with sleep
As we age, we are more likely to experience medical problems that can interfere with sleep. Take gastroesophageal reflux disease (GERD), diabetes, renal failure, respiratory diseases like asthma, and immune disorders, to name some common ones. As if having a health issue were not enough, some medicines can make it difficult to fall or stay asleep.
Our lives are also marked by change and other life events that can impact sleep. The death of a loved one, moving from a family home, physical limitations from age and illness, and psychological difficulties or psychiatric disorders can haunt our sleep.
Maintaining a daily routine is key
We all dream of owning our days once we retire. But we still need to establish a daily routine. Otherwise we risk disrupting our sleep schedules and invite problems.
- Be consistent with the time you go to bed and the time you wake. These should be in tune with your circadian rhythm.
- Get at least two hours of bright light during the day–it helps keep your circadian rhythm healthy.
- Exercise daily. Studies have shown that adults who exercise regularly take less time to fall asleep and get more sleep at night. But don’t exercise too late in the day–it acts as a stimulant and increases release of hormones like epinephrine and adrenaline.
- Avoid “blue light” exposure in the evening–it will trick your brain into thinking it’s still daytime. Blue light is emitted by electronics with screens, like smartphones and computers, as well as some energy-saving light bulbs. Exposure to light suppresses the secretion of melatonin.
- Watch your coffee/caffeine consumption. If you want a good night’s sleep stay away from caffeine after 3 or 4 p.m. Caffeine’s half life is about 6 hours–so about half of the caffeine from that one cup will still be in your system at 9 or 10 p.m. But few people are aware that caffeine has a quarter life–it takes another 5 or 6 hours for the remaining caffeine to reduce by half, contributing to restlessness overnight.
- Set your bedroom temperature between 60 and 67 degrees F. It will help your body to cool and initiate sleep. Sleep.org suggests thinking of your bedroom as a cave–dark, quiet, cool.
- Avoid alcohol and eating late in the evening. They can reduce production of melatonin and interfere with your circadian rhythm.
The best practice is to aim for at least 7 to 8 hours of sleep per night to lower the risk of heart disease and type 2 diabetes–and contribute to vitality in our 60s and 70s and beyond. Understanding how sleep works can help you formulate your own plan for wellbeing.
* * *
You may also like
- The power of a power nap
- Nine of the best anti-aging sunscreens for women
- Red in the face: We look at rosacea and treatments that work
Go to the Blue Hare home page for more articles for fabulous women.
